Data: The Beating Heart of Healthcare
Actian Corporation
August 4, 2021

Payers, health plans, and integrated health systems run on data. Integration, processing, and analytics are integral to their business process and managing of costs and risk.
The role of payers in the healthcare industry has been expanding for years. As care models have shifted from fee-for-service to coordinated and value-based care, payers and providers alike have been generating—and relying upon—more and more data to run operations smoothly. This evolution had been underway for some time, but the Covid-19 pandemic abruptly put new pressure on the system, heightening the need and requirements for better interoperability and data sharing between payers, providers, members, and patients.
Once, payers focused primarily on claims processing, payments, and plan membership management. But that was in a simpler time. Now, payers are focused on managing the relationship between members and providers and on delivering better patient health outcomes for members. They’re also focused on delivering better experiences for members and providers alike as new competitors are appearing on the horizon from unexpected sectors. Large organizations like Walmart, Amazon, and Google, are expanding their own operational profiles and starting to compete as payers in their own right. In some cases, these organizations are even taking on the role of healthcare providers and competing with traditional providers.
All these changes are putting considerable strain on payers. Add to these the erosion in commercial plan revenues—accelerated by Covid-19 through an uptick in self-care as well as increases in Medicaid and consumer direct purchasing of plans through the Affordable Care Act exchanges—which has reduced revenues and disrupted financial forecasting. During 2020, between 35 and 45% of Americans delayed or opted not to receive care, citing numerous concerns, including the pandemic-driven layoffs, both temporary and long-term, that hit many workers whose healthcare was tied to their employment.
Driving Better Outcomes With Data
To meet these challenges and to gain more predictability, to lower costs and risk while improving member and patient outcomes, organizations throughout the healthcare industry are trying to turn to data and analytics. According to a Society of Actuaries (SOA) survey, more than 90% of payer and provider executives say predictive analytics is key to effective healthcare management.
However, the goal of integrating the systems housing the relevant data and then deriving actionable insight from an analysis of this consolidated pool of data can be costly and elusive. IT is often overburdened, already tasked with integrating cumbersome legacy systems and data sources, including claims systems, walled-in provider data (EMR/EHR), connect operational systems (ERP), member and patient engagement (CRM) systems, external data such as SDOH, and new technologies such as wearables and virtual care systems. Nor are these long-needed integration projects the only demands weighing down IT. CMS and OMB are pressing ahead industry mandates to open up data access through newly finalized rules for data sharing—not only to patients but also across the healthcare ecosystem. Initially introduced by the Cares Act in response to Covid-19, these new rules require the industry to enable member access to data and facilitate interoperability between payers and health systems. Deadlines for compliance begin in 2021.
While these rules will, in theory, benefit payers, members, and providers by ensuring greater and more standardized access to data across the healthcare ecosystem, the work to achieve compliance can almost completely tie up an organization’s IT resources. This can make it even more difficult for data analysts, actuaries, and fraud and claims analysts to dive into these deep pools of data and extract actionable insights, because consolidating and accessing all this data in advance of analysis still requires the assistance of IT, which now has even less bandwidth to support users.
But there is a solution that can accelerate the integration and data sharing goals facing IT and that can enable an organization’s data scientists and analysts to consolidate and analyze critical healthcare data themselves, without having to heavily rely on the support of the IT team.
Enter the Healthcare Data Analytics Hub
The Actian Healthcare Data Analytics Hub enables payers, providers, and others in the healthcare ecosystem to gain greater insights and drive better outcomes with data. This SaaS-based hub includes native integration with the powerful data extraction, transformation, and load (ETL) features of Actian DataConnect, which enable an organization to automate and accelerate the process of accessing, pulling, and qualifying relevant data from a wide range of internal and external systems. Because connectors have already been built to link many of the systems and data repositories that healthcare organizations use, the integration work that IT has already begun becomes dramatically easier to complete. Similarly, the IT team can build the data access APIs described by CMS and ONC right in the Data Analytics Hub, ensuring that data can be shared securely and that member data sharing preferences can be both tracked and enforced across the healthcare data fabric, regardless of source or destination. The Actian Healthcare Data Analytics Hub also ensures that the IT organization can comply with the rules requiring that the systems and networks supporting both the sharing and protection of personal data stay on top of constantly evolving HIPAA and other regulatory requirements.
Beyond helping healthcare IT organizations to accelerate the completion of their integration and data sharing projects, the Data Analytics Hub can all but eliminate the need for an organization’s end users to petition IT for support when striving to perform their analytics. Self-service, native integration tools in the Actian Data Platform make it easy for healthcare data analysts, actuaries, provider network, revenue cycle management, and fraud and claims analysts to access and integrate data sets on their own, without help from IT—and without impacting the existing systems of record. The Actian Data Platform supports all popular analytic and visualization tools, so users can use the tools with which they are already familiar to gain the insights needed to automate and optimize processes, improve outcomes, and drive a more satisfying experience for all parties involved.
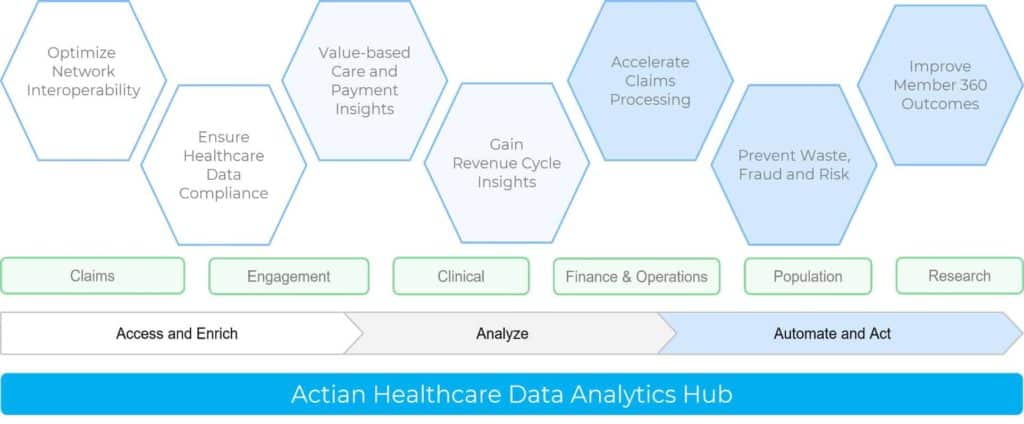
The result? Having an intelligent, end-to-end healthcare data analytics hub enables IT organizations to accelerate completion of the critical integration and data access projects they are already committed to completing. It also empowers an organization’s data scientists and analysts to perform the critical work that they have been tasked to perform by removing the roadblocks preventing them from gaining the insights they are trying to discover and act upon. An Actian Healthcare Data Analytics Hub enables an organization to shift from siloed models of business and operations to models that are forward-looking and collaborative. An organization can better manage the move to value-based care, find ways to compete more effectively against new competitors (many of whom are less burdened with a legacy IT infrastructure and can move nimbly in seizing new opportunities), improve the experiences of and alignment with members and partners alike, and, ultimately, improve outcomes, save time, and reduce costs.
About Actian
Actian has helped hundreds of payers, providers, clearinghouses, and healthcare technology organizations automate data integration, processing, and analysis, enabling them to capitalize on real-time analytics to derive essential insights and automate processes in an ever-evolving healthcare data landscape. Actian helps these organizations apply analytics and data processing to address a breadth of use cases from claims processing to population health insights and compliance.
Subscribe to the Actian Blog
Subscribe to Actian’s blog to get data insights delivered right to you.
- Stay in the know – Get the latest in data analytics pushed directly to your inbox.
- Never miss a post – You’ll receive automatic email updates to let you know when new posts are live.
- It’s all up to you – Change your delivery preferences to suit your needs.